Vasectomy and Immunologic Shifts
Introduction
Vasectomy is widely regarded as a safe, effective, and permanent form of male contraception. Over 500,000 vasectomy procedures are performed annually in the United States alone, with millions more worldwide. Despite its routine nature, growing attention is being paid to the biological aftermath of vasectomy—especially the subtle, often overlooked, immunologic shifts that may follow the procedure.
This article explores the immune responses triggered by vasectomy, examines their clinical relevance, and discusses ongoing debates surrounding autoimmune sequelae and long-term systemic effects.
The Immune Landscape Before Vasectomy
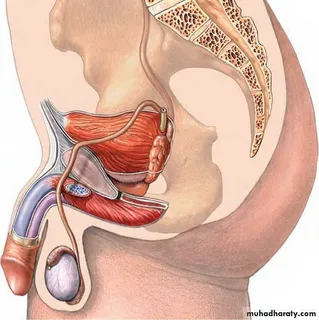
The male reproductive system is uniquely protected from immune surveillance. The blood-testis barrier functions to prevent immune cells from recognizing and attacking developing sperm cells, which are immunogenic due to their post-puberty antigenic profile. The testes, epididymis, and associated ducts are considered “immunoprivileged” zones.
This immune isolation is crucial because spermatozoa contain surface proteins that the immune system would interpret as foreign. The body’s self-tolerance mechanisms do not account for these antigens since they emerge after central immune education in the thymus.
What Happens Immunologically After Vasectomy?
Vasectomy disrupts this delicate immune equilibrium. During the procedure, the vas deferens—the duct that transports sperm from the epididymis to the ejaculatory duct—is severed or sealed. This blockage leads to sperm accumulation and eventual leakage into the interstitial tissue, especially if pressure builds up.
Once sperm leak into surrounding tissue, they come into contact with immune cells, setting off a cascade of responses. The most prominent shifts include:
1. Anti-sperm Antibody (ASA) Formation
One of the hallmark immunologic shifts post-vasectomy is the development of anti-sperm antibodies. In up to 60-80% of men, the immune system mounts a response to sperm antigens, producing IgG, IgA, and sometimes IgM antibodies.
These ASAs can:
- Bind to sperm heads or tails, affecting motility.
- Impede sperm-egg fusion.
- Lead to agglutination (clumping).
While this antibody formation has little relevance for men not seeking fertility restoration, it becomes a critical issue during vasectomy reversals or assisted reproduction attempts.
2. Local Inflammatory Reactions
Leaked sperm can provoke localized immune activity, including granuloma formation. A sperm granuloma is a benign, chronic inflammatory response to extravasated sperm. Macrophages and T-cells accumulate at the site, creating a small nodule.
Though usually asymptomatic, granulomas serve as evidence of the body treating sperm as foreign invaders, resulting in cell-mediated immune activation. In rare cases, these granulomas can cause discomfort or chronic inflammation.
3. Systemic Immune Activation
While most immune activity remains localized, some researchers have noted elevated systemic inflammatory markers post-vasectomy. Elevated cytokines such as IL-6, TNF-α, and IFN-γ have been found in certain studies. However, clinical significance remains inconclusive.
These low-grade immunologic responses have fueled speculation about vasectomy’s possible link to autoimmune diseases, though large-scale epidemiologic studies have not confirmed consistent associations.
Is Vasectomy Linked to Autoimmune Disease?
The debate surrounding vasectomy and autoimmune disease—particularly rheumatoid arthritis, multiple sclerosis, and lupus—has persisted for decades. Some small-scale studies have shown modest associations, but comprehensive meta-analyses largely refute a strong causal relationship.
What complicates matters is that autoimmune disorders tend to be multifactorial. Genetic predisposition, environmental exposures, infections, and hormonal factors all contribute. Vasectomy, if contributing at all, likely plays a minor or conditional role.
Vasectomy and Immune Privilege Breakdown
One of the more profound immunologic consequences of vasectomy is the disruption of immune privilege in the testes. Breaching the blood-testis barrier can expose immune cells to a range of sperm-specific antigens. This can result in:
- T-cell sensitization
- Antigen-presenting cell activation
- Altered testicular cytokine milieu
While this immune breach is typically well-managed by the body’s compensatory mechanisms, in a small subset of men, it could lead to chronic orchitis (testicular inflammation), testicular atrophy, or idiopathic infertility—even in cases where vasectomy reversal is performed.
Implications for Vasectomy Reversal
For men seeking vasectomy reversal, immunologic shifts present a real challenge. Even after re-establishing patency through vasovasostomy or vasoepididymostomy, anti-sperm antibodies can impair fertility outcomes.
Key observations:
- High titers of ASAs are correlated with lower post-reversal pregnancy rates.
- Assisted reproductive techniques (like IVF with ICSI) often bypass these issues.
- Screening for ASAs is occasionally recommended in the pre-IVF evaluation.
Thus, vasectomy may initiate long-term immune responses that persist even when anatomical continuity is restored.
Vasectomy and Chronic Pain: An Immunologic Basis?
Post-vasectomy pain syndrome (PVPS) affects a small percentage of men but remains a challenging and poorly understood condition. While nerve injury and congestion have been implicated, immune-mediated inflammation may also play a role.
T-cell infiltration, macrophage activation, and elevated local cytokines could sensitize nerves, perpetuating chronic scrotal pain. Emerging data suggests that immunomodulatory therapies might eventually become part of PVPS management.
Animal Studies and Experimental Evidence
Animal models have offered critical insight into vasectomy-induced immunologic shifts. In vasectomized rodents and primates:
- Autoimmune orchitis is more common than in humans.
- Testicular degeneration is accelerated in some strains.
- Gene expression profiles of immune response genes are altered.
These models support the concept that vasectomy induces immunologic remodeling, though species-specific differences in immune privilege mechanisms limit direct applicability.
Clinical Perspective: Should Immune Effects Influence Decision-Making?
From a clinical standpoint, vasectomy remains an overwhelmingly safe procedure with minimal long-term health risks for the majority of men. Nonetheless, informed consent should include mention of:
- The possibility of anti-sperm antibody formation
- Challenges in future fertility restoration
- The rare chance of chronic pain syndromes with possible immune contributions
In men with autoimmune predispositions or fertility preservation concerns, sperm banking prior to vasectomy is a prudent step.
The Future: Biomarkers and Personalized Vasectomy Counseling
With advances in immunogenetics and molecular diagnostics, the future may hold:
- Pre-vasectomy immune profiling to identify at-risk individuals
- Cytokine biomarker panels to monitor post-vasectomy inflammation
- Personalized reversal strategies based on ASA titers and T-cell assays
Artificial intelligence (AI) and machine learning could also assist in modeling immunologic outcomes and long-term fertility predictions post-vasectomy.
Conclusion
Vasectomy is more than a mechanical disconnection of sperm transport—it triggers a cascade of immunologic shifts that reflect the body’s complex response to sperm antigen exposure. While generally benign, these responses have meaningful implications for reversal outcomes, long-term fertility, and a small subset of post-vasectomy complications.
Ongoing research into testicular immunology, sperm autoimmunity, and immune-privilege disruption will continue to refine how we counsel patients and manage the downstream effects of vasectomy. Understanding these immunologic shifts is crucial for clinicians, researchers, and patients navigating the landscape of male reproductive health.
FAQs
1. Can vasectomy cause autoimmune disease?
While vasectomy can lead to the formation of anti-sperm antibodies and local immune activation, current large-scale studies do not support a strong link between vasectomy and systemic autoimmune diseases like lupus or rheumatoid arthritis.
2. Will a vasectomy affect my immune system overall?
Vasectomy may result in localized immune changes, such as anti-sperm antibody formation and mild inflammatory responses. However, it does not significantly impair or alter systemic immunity in most men.
3. Are there tests to check for immune issues after vasectomy?
Yes. Testing for anti-sperm antibodies (ASA) can be done through semen analysis or blood tests. These tests are most relevant if you’re considering vasectomy reversal or encountering fertility issues afterward.